After having a baby, Erin began experiencing pain in her lower back and was leaking urine with some activities. She felt like she was sitting on a golf ball. She figured these symptoms would go away over time, so she kept them to herself. But the symptoms didn’t go away, and Erin wondered how she would continue living this way.
But Erin’s story isn’t some one-off situation or something that would dissolve into the catalog of rare side effects of pregnancy.
Erin’s experience isn’t rare, nor is it exclusive to women who have given birth. Additionally, according to the International Urogynecological Association (IUGA), up to 40% of women have a minor degree of prolapse with minimal to no symptoms. Either way, prolapse is somewhat common and pelvic floor rehab is an excellent, first-line conservative option for treatment! It is something our pelvic floor specialists, like Molly Nelson, DPT, CLT, see plenty of. Every day.
What is Pelvic Organ Prolapse?
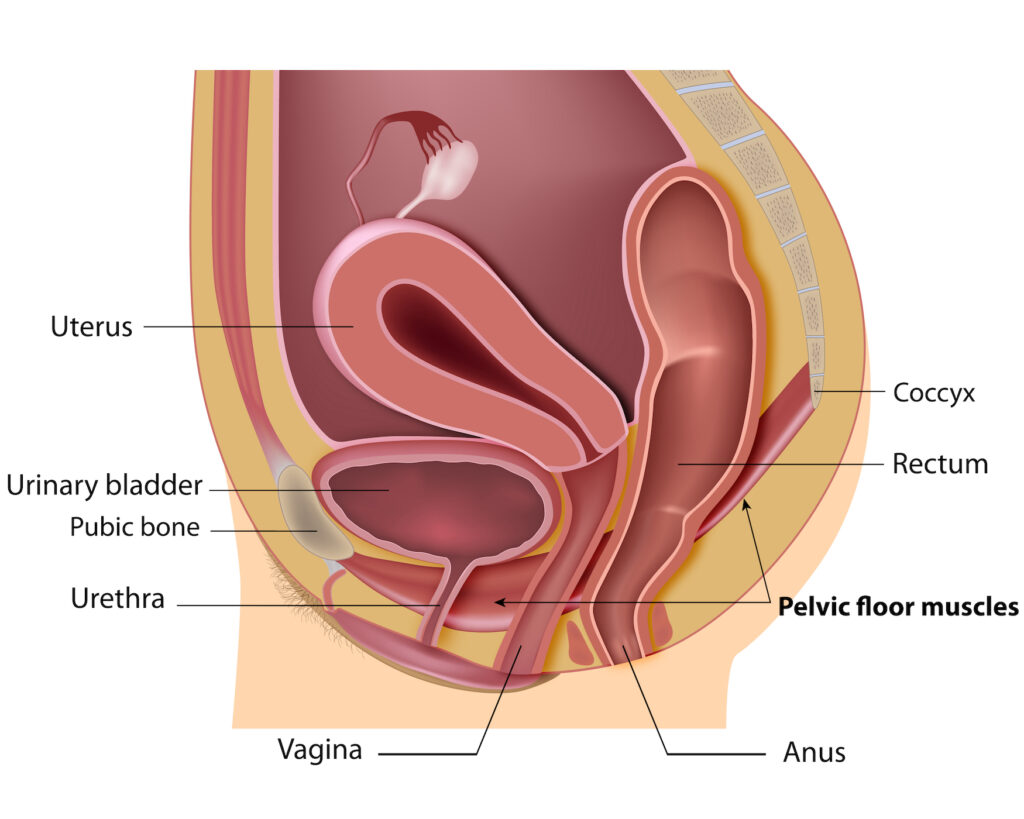
Think of your pelvic muscles and tissues as a hammock that supports your pelvic organs. These organs include the bladder, uterus and cervix, vagina, and rectum. When the support structure weakens, the organs cause a protrusion into or out of the vagina.
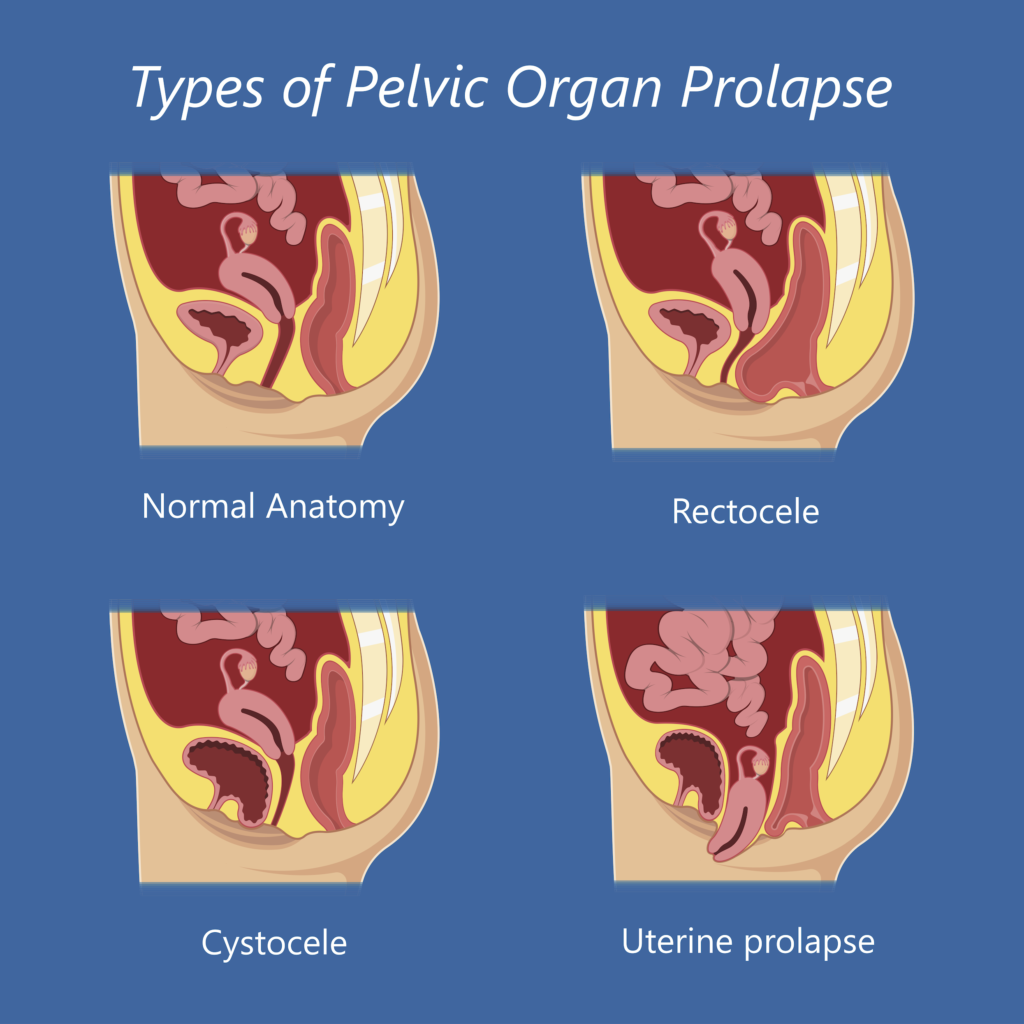
There are four different types of pelvic organ prolapse. The name varies by the organ that is affected.
- Cystocele – The most common type of prolapse occurs when the bladder, behind the front vaginal wall, bulges into the vagina.
- Rectocele – This happens when the rectum, behind the back vaginal wall, bulges into or out of the vagina.
- Uterine Prolapse – This occurs when the uterus, at the top of the vagina, protrudes down into or out of the vagina.
- Enterocele – Less common than the others, the intestines can descend between the other pelvic organs towards the vaginal opening, typically between the vagina and the rectum.
Symptoms of Prolapse
The most common symptoms of prolapse include changes in bladder and bowel habits. This can mean more frequent bathroom visits, urgency – the need to go now, difficulty emptying the bladder, recurrent bladder infections, heaviness in the bladder, and vaginal pressure that may worsen with activity or throughout the day. Pain can also be a symptom, but not exclusively.
Causes of Prolapse
The most common risk factors for prolapse include:
- Childbirth
- Age
- Hormonal changes caused by menopause
- Family history
- Cancer
- Aging and collagen malformation
- Chronic straining/coughing/constipation
How Pelvic Organ Prolapse is Treated
Depending on the type of prolapse and its severity, treatment recommendations can vary. Pelvic floor physical therapy is often the first treatment recommended. This is because by strengthening the pelvic floor, they can better support the pelvic organs. The challenge is that a large number of people do Kegels incorrectly. If a person doesn’t know what muscles to squeeze, how will they do a proper Kegel? Molly is specially trained to help her patients identify and isolate the correct muscles.
“What a patient puts into pelvic floor physical therapy is what they will get out of it,” said Molly.
A level of commitment and follow-through is necessary for this treatment option to work. Therapy, on average, takes four to six visits over a couple of months to complete. But between visits and after therapy has ended, patients are required to do their pelvic floor exercises and other strengthening regularly.
While this is the most utilized treatment option for prolapse, it isn’t for everyone. Physical therapy won’t reverse the prolapse but will strengthen the supportive structures, so the symptoms abate.
Sometimes the use of a pessary is helpful. A pessary is a specially made, removable device made of silicone inserted into the vagina to support the prolapsed organ. A pessary also can help a woman perform Kegels.
Surgery may also be an option depending on the severity of the prolapse and symptoms associated. A consultation with a physician to learn about options may be appropriate. A pelvic floor therapist can facilitate this.
How to Prevent Prolapse
Molly’s biggest advice for preventing pelvic organ prolapse is to treat the pelvic floor just like any other muscle and give the pelvic floor and general strengthening some attention regularly. Pelvic floor rehab can tailor a pelvic floor and comprehensive strengthening program to maintain overall pelvic health.
“Women who are pregnant or plan to become pregnant should build a strong pelvic floor foundation before childbirth,” said Molly.
And for older women, well, here’s a reality check for you; the insides age just like the outsides. Skin becomes less taut and thinner, causing wrinkles and drooping. The same is true for your insides.
“In general, everything heads south – including pelvic organs.,” said Molly. “The pelvic floor tissue becomes thin and fragile, which can add insult to injury.”
She recommends that women focus on being stronger each decade of their life as it takes more time to build up strength. And for Molly, she plans to go into her 40s stronger than her 30s. To help make that possible she maintains a comprehensive strengthening program with her Kegels.
As for Erin, she is now pain-free and has gone back to her favorite sport of running, without leaking and that golf ball pressure, no less.
