Should pelvic floor therapy be a part of your postpartum care?
The answer to that question is probably YES! If you had a vaginal delivery or even a cesarean birth then your pelvic floor muscles are likely in need of some rehabilitation. You might be asking yourself what is the pelvic floor and why would it need rehab? Great questions.
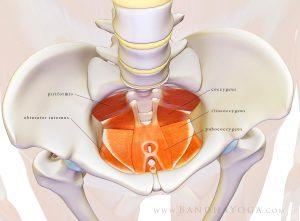
Lastly, the pelvic floor provides stability to our trunk. Along with the diaphragm, abdominal wall, and muscles in our back called multifidi, the pelvic floor contracts during functional movements becoming a sturdy canister for the rest of our body to move off of. It’s pretty amazing that such a small group of muscles can provide so many important functions.
Here’s the important part for you postpartum ladies out there: Because the pelvic floor can experience massive stretch, tearing, and incisions called episiotomies, during childbirth they can lose their ability to function properly. This means that postpartum women are more likely to experience urinary leakage, pelvic organ prolapse, and pelvic pain. In fact, one study found that 92% of postpartum women report urinary leakage 12 weeks after delivery. When these same women were asked again 5 years later 92% of them continued to experience leakage (Viktrup et al 2000). As for pelvic organ prolapse, 50% of women who have experienced childbirth have some degree of prolapse (Hagen & Stark 2001). Prolapse can be accompanied with symptoms of pelvic heaviness, backache, and vaginal bulging.
So what is pelvic floor therapy and how can it help?
As pelvic floor therapists we have special training to assess the pelvic floor through an internal vaginal assessment, or if someone is not comfortable with this then we can assess their pelvic floor with external techniques. We assess the pelvic floor for strength, coordination, and endurance. This helps us figure out why someone might be experiencing leakage, pain, or prolapse. Often times we find that a woman is doing a pelvic floor contraction (A.K.A “kegel”) incorrectly. An incorrect contraction can look differently depending on the person. Some women squeeze accessory muscles in their butt, thighs, and abdomen instead of the pelvic floor. Other women actually bear down utilizing a valsalva movement instead of doing a kegel. This can actually worsen symptoms like prolapse and urinary incontinence. In these cases, we teach them how to do a kegel the correct way so that they can strengthen their pelvic floor in isolation. We then teach them how to coordinate the pelvic floor muscles with activities such as sneezing, coughing, jumping, running, etc. so that they don’t experience leakage or prolapse during these activities.
Thankfully in the US, pelvic floor therapy is becoming more recognized however this modality is still underutilized in postpartum care compared to other countries. Often times medication and surgery are the first line of treatment for these issues, which is unfortunate when a more conservative and effective treatment exists.
The pelvic floor therapists at Alpine Physical Therapy are hopeful of a future where pelvic floor therapy becomes a cornerstone in every woman’s postpartum care. If you are a postpartum woman in any stage, whether you had a baby 6 weeks ago or 6 years ago, you could benefit from this form of physical therapy for prevention and treatment of pelvic floor issues.
If you have any further questions or inquiries call Alpine at 541-382-5500 or email emily@alpinephysicaltherapy.com
References
- Viktrup L, Lose G. Lower urinary tract symptoms 5 years after the first delivery. Int Urogynecol J Pelvic Floor Dysfunct 2000;11:336–40.
- Hagen, S. and Stark, D. Conservative prevention and management of pelvic organ prolapse in women. Cochrane database of systematic reviews, 2011, 12, CD003882

There are some wonderful places where we can go. After the observation of some places are very attractive. We can see charming views at some places. We can capture some beautiful views which can be memorable.
I had no idea that the pelvic floor could be damaged so much during child birth. My friend recently had a baby, so I think she’d really benefits from reading this. Do you have any tips for finding a good physical therapist in her area to help her?
I realized that pelvic floor physiotherapy should be a part of my postpartum care since I might have suffered prolapse. It’s a good thing that it can help me assess why I am suffering prolapse as you stated since I am having trouble conceiving. Since you mentioned that vaginal bulging could be a sign of it, a therapist should hopefully help me regain the muscles I need to use to have a second child.